Dr. Domb is a nationally recognized orthopedic surgeon specializing in sports medicine and regenerative medicine. He is proficient in arthroscopic surgery of the knee, including meniscus repair and ACL reconstruction.
- Knee Basics
- Knee Injuries & Conditions
- Non-surgical & Regenerative Medicine
- Surgeries Performed by Dr. Domb
Knee Anatomy

- The knee is classified as a hinge joint and is comprised of three bones: the femur, patella and tibia. The fibula, or non-weight bearing lower leg bone, is located nearby. Several muscles, tendons and ligaments support the knee joint. Each structure provides support and permits motion of the knee joint including flexion, extension and subtle rotation of the lower leg.
- The quadriceps muscle group is a set of 4 muscles located on the anterior aspect of the thigh that assist in knee extension and hip flexion. The antagonist muscle group to the quadriceps is the hamstrings; three muscles located on the posterior aspect of the thigh assisting in knee flexion.
- There are four ligaments within the knee joint. The anterior (ACL) and posterior (PCL) cruciate ligaments crossover deep within the knee and are the largest ligaments in the joint. The ACL prevents the tibia from sliding forward, while the PCL prevents the tibia from sliding backward away from the femur. The medial collateral (MCL) and lateral collateral (LCL) ligaments are found on the inside (medial) and outside (lateral) aspect of the knee respectively. They prevent the knee from bending sideways in either direction.
- The meniscus consists of two connected semi-circular rings of cartilage located between the femur and the tibia. The menisci are located medially and laterally, providing stability as the knee bears weight and pivots. The medial meniscus is partially attached to the MCL, thus concurrent injuries in these two soft tissues often occur. There is no connection between the lateral meniscus and LCL.
- Articular cartilage is also present on the ends of the bones within the joint, acting as a cushion between the bones. Synovial fluid, or fluid within the joint, also helps to reduce friction and allows the bones of the joint to move smoothly.
- The two major tendons of the knee are connected to the patella, commonly referred to as the kneecap. The tendon inferior (below) to the patella is the patellar tendon, which connects the patella to the tibia. The tendon superior (above) to the patella is the quadriceps tendon, which connects the quadriceps muscle to the patella. The quadriceps tendon, patella and patellar tendon form a pulley system to create the extensor mechanism of the lower leg and knee.
Publications by Dr. Domb on Knee Basics
- Magnetic Resonance Imaging of the Knee 2001
- Magnetic Resonance Imaging of the Knee Current Techniques and Spectrum of Disease 2006
- Radiographic Evaluation of Pathologic Bone Lesions - Current Spectrum of Disease and Approach to Diagnosis 2004
- Toe walking 2004
Get Adobe ReaderYou will need the Adobe Reader to view & print these documents.

Meniscal Tears
The role of the meniscus is to provide cushion, act as a shock absorber and prevent extreme pivoting of the knee. Meniscal tears are among the most common knee injuries. Many athletes, especially runners and those in contact sports, are highly susceptible to tears. However, individuals at any age can experience tearing of the meniscus.

ACL Injuries
The ACL (anterior cruciate ligament) is the main support structure of the knee joint. It prevents forward translation of the tibia relative to the femur. The ACL is the most common injured ligament in the knee. Injuries to the ACL are typically caused my traumatic events such as collisions in athletics, accidents or severe falls.

Patellar Dislocations
Patella, or kneecap, dislocations can occur with extremes of knee pivoting and rotation. Generally this involves the patella slipping laterally, or to the outside of the knee. After the first dislocation, conservative measures are pursued including rest, bracing, physical therapy and anti-inflammatories.

Chondral Defects
A chondral defect refers to damage to the articular cartilage located at the end of bones. Specific to the knee joint, damage can occur at the distal end of the femur (thigh bone), the proximal tibia (lower leg bone), or the posterior aspect of the patella (knee cap).

Loose Bodies
A loose body is a small piece of cartilage or bone that is floating within the joint. These often result from injury or severe muscle strain at the muscular insertion. Loose bodies can cause sharp pain and may even cause a person to feel their joint give way. Certain conditions such as synovial chondromatosis of the hip may cause multiple loose bodies within the joint.

Osteoarthritis
Osteoarthritis is degenerative in nature; considered chronic destruction of the articular cartilage of the joint. As cartilage is worn down, bones within the joint rub together, causing pain, swelling and stiffness.

Knee Tendonitis
Tendonitis refers to the swelling and irritation of the tendons surrounding the knee. Patellar tendonitis is the most common knee tendonitis. Fast growing adolescents and older populations are at an increased risk of this condition.

Other Knee Ligament Injuries
The MCL (medial collateral ligament) and LCL (lateral collateral ligament) are located at the medial (inner) and lateral (outer) aspects of the knee, respectively. These ligaments work with the ACL and PCL to keep the knee stable during motion and activity.
Physical Therapy

Physical therapy can provide strengthening and conditioning of a joint to compensate for an injury. Physical therapists often provide varying modalities for treatment of injuries, including assisted stretching, massage and strengthening. Physical therapy is also a useful tool in retraining a joint after surgery. It is highly effective in facilitating an athlete to return to sport in a safe manner.
Ultrasound Guided Injections
Dr. Domb and his team are highly trained in ultrasound-guided injections. These procedures are performed in the office at the time of your visit. The ultrasound machine assists Dr. Domb and his Physician Assistants to safely place injectable medications into the joint. Knee injection options include:
- Cortisone: A combination of steroid medication and local anesthetic to provide pain relief and decrease inflammation caused by intra-articular injury or arthritis. A patient can have a cortisone injection every 3-4 months.
- Synvisc: Synvisc is considered a viscosupplementation, indicated for patients who have failed conservative management of osteoarthritis. The injection consists of purified animal cartilage designed to act as a lubricant to the joint. Synvisc can be given once every 6 months.
Platelet Rich Plasma (PRP)
PRP is an injection of your own platelets & growth factors, similar to orthobiologics treatment, extracted from your blood. The blood draw & injection are done at the same office visit, an outpatient clinical procedure.
PRP has shown great promise in stimulating repair of body tissues including tendons, ligaments & cartilage. PRP mimics the body's innate response to an injury by stimulating platelet activation. The activation of platelets plays a dynamic role in soft tissue healing. Research shows that PRP is superior to other injections in the treatment of osteoarthritis and healing of chronic tendinitis.
In osteoarthritis, PRP can enhance the body's normal healing response in an acute manner for a chronic condition. This can result in the development of new collagen, a benefit that other injections are unable to offer.
In tendinitis, the growth factors in PRP can signal the body to initiate a healing response in the local injected tissues. Healing is the first step in injured tissues regenerating their strength and function. It has been used extensively in professional athletes who seek hurried return to play. Star athlete success stories include: Kobe Bryant (NBA), Tiger Woods (PGA tour), Alex Rodriquez (MLB), Hines Ward (NFL) and Rafael Nadal (ATP).
If you have an injury or condition involving a tendon, ligament, joint or osteoarthritis, PRP may be a nonsurgical option for you.
Indications (including but not limited to):
- Osteoarthritis (Intraarticular)
- Tendinosis & Tendinitis
Process
- 3 Injections spaced 1 week apart x 3 weeks
- Can have injection series every 6 months
- Day of Injection
- Blood Draw
- Centrifuge x 5 minutes
- Ultrasound Guided Injection
- Cortisone: A combination of steroid medication and local anesthetic to provide pain relief and decrease inflammation caused by an intra-articular injury or arthritis. A patient can have a cortisone injection every 3-4 months.
- PRP and Tendinitis
- PRP and Hip Osteoarthritis
- PRP versus Viscosupplementation in Osteoarthritis
- PRP and Knee Arthritis
orthobiologics Therapy
orthobiologics therapy is a form of regenerative medicine that utilizes the body’s natural healing mechanism to treat various conditions.
orthobiologics are being used in regenerative medicine to renew and repair diseased or damaged tissues and have shown promising results in treatments of various orthopedic, cardiovascular, neuromuscular and autoimmune conditions.
orthobiologics are present in all of us acting like a repair system for the body. However, with increased age sometimes the optimum amount of orthobiologics are not delivered to the injured area. The goal of orthobiologics therapy is to amplify the natural repair system of the patient’s body.
Types of orthobiologics
There are two major types of orthobiologics embryonic orthobiologics and adult orthobiologics. Embryonic orthobiologics (ESCs) are orthobiologics derived from human embryos. They are pluripotent, which means they have the ability to develop into almost any of the various cell types of the body.
As the embryo develops and forms a baby, orthobiologics are distributed throughout the body where they reside in specific pockets of each tissue, such as the bone marrow and blood. As we age, these cells function to renew old and worn out tissue cells. These are called adult orthobiologics or somatic orthobiologics. Like embryonic orthobiologics, adult orthobiologics can also replicate into more than one cell type, but their replication is restricted to a limited number of cell types.
Use of orthobiologics in Orthopedics
The unique self-regeneration and differentiating ability of embryonic orthobiologics can be used in regenerative medicine. These orthobiologics can be derived from eggs collected during IVF procedures with informed consent from the patient. However, many questions have been raised on the ethics of destroying a potential human life for the treatment of another.
Adult orthobiologics are most commonly obtained from the bone marrow, specifically the mesenchymal orthobiologics, which have the ability to replicate into cells that form the musculoskeletal system such as tendons, ligaments, and articular cartilage. They can be obtained from the iliac crest of the pelvic bone by inserting a needle and extracting the orthobiologics from the bone marrow.
Currently, orthobiologics therapy is used to treat various degenerative conditions of the shoulder, knees, hips, and spine. They are also being used in the treatment of various soft tissue (muscle, ligaments and tendons) as well as bone-related injuries.
Who is a Good Candidate for a orthobiologics Procedure?
You may be a good candidate for orthobiologics therapy if you have been suffering from joint pain and want to improve your quality of life while avoiding complications related to invasive surgical procedures.
Preparing for the Procedure
- It is important that you stop taking any non-steroidal anti-inflammatory drugs (NSAIDs) at least two weeks before your procedure.
- Preparing for a orthobiologics procedure is relatively easy and your doctor will give you specific instructions depending on your condition.
orthobiologics Procedure
The procedure begins with your doctor extracting orthobiologics from your own bone marrow. Bone marrow is usually aspirated from your hip region. Your doctor will first clean and numb your hip area. A needle is then introduced into an area of your pelvic bone known as the iliac crest. Bone marrow is then aspirated using a special syringe and the sample obtained is sent to the laboratory. In the laboratory, the aspirate is spun in a machine for 10 to 15 minutes and a concentrated orthobiologics sample is separated.
Your doctor then cleans and numbs your affected area to be treated and then, under the guidance of special x-rays, injects the orthobiologics into the diseased region. The whole procedure usually takes less than one hour and you may return home on the same day of the procedure.
Post-Operative Care
- You will most likely be able to return to work the next day following your procedure.
- You will need to take it easy and avoid any load bearing activities for at least two weeks following your procedure.
- You will need to refrain from taking non-steroidal, anti-inflammatory medications (NSAIDS) for a while as this can affect the healing process of your body.
Advantages & Disadvantages
- orthobiologics therapy is a relatively simple procedure that avoids the complications associated with invasive surgical procedures.
- As orthobiologics therapy uses the cells derived from your own body it reduces the chances of an immune rejection.
Disadvantages
- The disadvantage of adult orthobiologics therapy is lack of data about its long-term effects as it is a newer evolving therapy.
Risks and Complications
orthobiologics therapy is generally considered a safe procedure with minimal complications, however, as with any medical procedure, complications can occur.
Some risks factors related to orthobiologics therapy include infection as the orthobiologics may become contaminated with bacteria, viruses or other pathogens that may cause disease during the preparation process.
The procedure to either remove or inject the cells also has the risk of introducing an infection to the damaged tissue into which they are injected. Rarely, an immune reaction may occur from injected orthobiologics.
Get Adobe ReaderYou will need the Adobe Reader to view & print these documents.
Arthroscopic Repair of the Knee
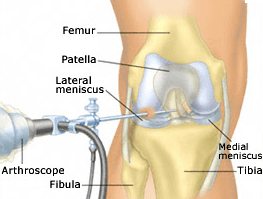
Arthroscopic knee surgery incorporates the use of small poke-hole incisions (portals) around the joint, and the use of a specialized camera (arthroscope) among other specified arthroscopic surgical instruments. The goal of arthroscopic surgery is to repair and restore the joint to optimal strength, while maintaining range of motion. Due to the minimally invasive nature of the arthroscopic technique, damage to surrounding muscles, ligaments, tendons, nerves and blood vessels is significantly reduced. Risk of infection, post-operative pain and rehabilitation are also decreased compared to the traditional open-technique. Knee arthroscopy can accomplish both diagnostic and therapeutic results.
All knee arthroscopy patients can expect to be involved in physical therapy after surgery to strengthen and condition their knee and return to sports in peak condition.
ACL Repair and Reconstruction
- ACL surgery involves the removal of damaged ligament fragments and replacement of the ligament with either the patient's own soft tissue or tissue from a cadaver; known as an autograft or an allograft respectively. ACL surgery may either be performed as an outpatient, or inpatient procedure with an overnight hospital stay.
- Recovery After an ACL reconstruction, patients can expect to bear weight as tolerated without a brace as long as there were no other injuries to the knee requiring additional surgical intervention. They may use crutches for the initial days of recovery to regain stability during ambulation. The patient will also use a continuous passive motion machine daily to prevent stiffness postoperatively.
Meniscus Repair and Meniscectomy
- Large meniscal tears and tears that fail to improve with conservative measures may require surgery. Surgery for a torn meniscus is an outpatient, arthroscopic procedure. The goal of the surgical procedure is conserve as much of the meniscus as possible. If the torn portion of the meniscus is removed from the knee, it is referred to as a partial meniscectomy. If the meniscus if can be repaired, the torn edges of the meniscus will be reattached with sutures or tacks.
- Recovery After a meniscectomy, a patient can expect to bear weight as tolerated and expect to not wear a brace, unless they have experienced an additional injury.After a meniscal repair, a patient can expect to have restricted weight bearing and use crutches for 2-6 weeks. This protects the repair during the early healing phases.
Recurrent Patellar Dislocation Surgical Repair
- Patella, or kneecap, dislocations can occur with extremes of knee pivoting and rotation. Generally this involves the patella slipping laterally, or to the outside of the knee. After the first dislocation, conservative measures are pursued including rest, bracing, physical therapy and anti-inflammatories. A severe dislocation causes disruption of the medial patellofemoral ligaments, which act to stabilize the patella. If this injury becomes recurrent and the patient has continued instability of the knee, arthroscopic surgical intervention may be necessary to repair the Medial Patellofemoral Ligament.
- Recovery After a MPFL reconstruction, the patient can expect to have restricted weight bearing and crutches for approximately 6 weeks. Patients can also expect to be in a knee brace for approximately 6 weeks.
Other Knee Surgeries
Quadriceps or Patellar Tendon Rupture Repair
-
Severe traumatic injuries can cause rupture to the quadriceps or patellar tendon. Quad tendon ruptures are more common in patients over 40 years old, while the majority of patellar tendon ruptures are seen in patients younger than 40 years old. As the extensor mechanism of the knee has been disrupted, patients generally have severe difficulty bearing weight on the leg or holding the leg straight. Severe tears will require open surgical intervention for repair.
- Recovery After a quadriceps or patellar tendon reconstruction, the patient can expect to have restricted weight bearing and crutches for approximately 6 weeks. Patients can also expect to be in a knee brace for approximately 6 weeks.
- All knee tendon repair patients can expect to be involved in physical therapy after surgery to strengthen and condition their knee and return to sports in peak condition.
Microfracture of the Knee
The smooth movement of the knee is attributed to articular cartilage, a smooth tissue that lines the bones of the joint, acting as a shock absorber and reducing friction when the bones glide over each other. Wear and tear and injury of the cartilage can lead to pain and impaired function. Since it is a complex avascular tissue and has no blood supply, it is unable to repair itself. Microfracture is a procedure performed to repair damaged knee cartilage by drilling small holes into the knee joint to create a new blood supply and stimulate new cartilage growth.
Microfracture is performed under local, spinal or general anesthesia. A small incision is made on your knee to insert an arthroscope, a narrow tube with a tiny camera at its end that enables clear visualization of the inside of your joint. Another incision is made through which specially designed instruments are inserted. Your surgeon prepares the area by removing any damaged cartilage. Multiple tiny holes called microfractures are then made into the subchondral bone (below the cartilage) with a sharp tool called an awl. This helps to bring blood supply from the deeper more vascular bone to the surface tissues. This technique creates a nourishing environment for tissue regeneration by using the body’s natural healing abilities to form new cartilage.
Following microfracture, your surgeon will recommend physical therapy to help restore motion of the operative joint. Immediately after the surgery, most patients can begin physical therapy with a continuous passive motion machine or CPM. You will be instructed on using crutches to avoid weight bearing activities for a few days. You will be allowed to return to sports or other intense activities 4 months after surgery.



